Elizabeth Adamson, Edinburgh Napier University, UK
Healthcare provision is under increasing pressure as people are living for longer and many with long term conditions who require ongoing treatment and care (Stucki, Bickenbach, Gutenbrunner, & Melvin, 2018). Compassion continues to be central to the provision of excellent care (McSherry, Timmins, de Vries, & McSherry, 2018) and how patients are cared for is as important to them as the nature of the care itself (Dewar & Nolan, 2013; Edinburgh Napier University & NHS Lothian, 2012). Despite this realisation and associated increased emphasis on provision of compassionate care globally (Dewar & Nolan, 2013; MacArthur, Wilkinson, Gray, & Matthews-Smith, 2017), even the most vulnerable people do not always experience this (McSherry et al., 2018; Parliamentary Health Service Ombudsman, 2011). Reports of poor care have featured in the press (Sinclair et al., 2016), resulting in calls for action such as careful screening of student nurse candidates for a compassionate disposition (Timmins & de Vries, 2015). Research shows that health professionals enter the profession with the intension to care (Mackintosh, 2006). Unfortunately, not all care environments are conducive to this and through the sociocultural influences in practice nurses can become desensitised to patient need (McSherry et al., 2018). Students may be encouraged to keep their distance from those for whom they care in order to protect themselves (Dewar, Adamson, Smith, Surfleet, & King, 2014). Although nurse educators are rarely able directly to ameliorate the significant practical challenges their students will encounter in healthcare environments, they can do much to prepare developing practitioners to work effectively within them.
Patients associate quality care with connectedness, attentiveness to patient comfort and kindness (Grimley, 2017). They value nurses detecting and attending to the little things that matter most to them and treating them as a person not a number (Adamson, Pow, Houston, & Redpath, 2017). Nurses need to identify and work adaptively with the constantly arising variations in circumstances, conditions and the people for whom they care and students need explicit and sustained support to learn how to do this. This paper suggests that one way to help nursing students is to support them develop an ethic of craftsmanship, underpinned by the key abilities and characteristics associated with this. This ethic involves a commitment to work that is excellent (Berger, 2003; Coeckelbergh, 2014).
In the widening access agenda and broad entry gate to education, student nurses embark on their programme of study with a range of life experience, differing values and beliefs and varying degrees of sensitivity to the needs and feelings of others. It is unwise to assume that students are naturally caring and that compassion is entirely innate. Research shows that curriculum can emphasise knowledge-based competencies which can dominate students’ attention, to the detriment of compassionate caring (Sinclair et al., 2016). Therefore, a key challenge for educators is to explicitly and sympathetically provide the tools, opportunities and environment for students to develop not only compassionate caring skills but attributes of craftsmanship, such as development of tacit knowledge and a commitment to do a good job for its own sake regardless of circumstances.
Prompted by Sennett’s (2008) seminal work on craftsmanship, Meal and Timmons (2012) call for Craftsmanship in nursing to be ‘Reclaimed’. The notion of the Art and Craft of nursing in general has been widely debated (Edwards, 1998; Jenner, 1997; LeVasseur, 1999) but not explicitly applied to the aspect of compassionate caring, much of which I argue resides in tacit knowledge and is a key feature of my model.
Tacit knowledge is closely associated with craftsmanship. Sennet’s work is founded on educational approaches that enable students to develop this for themselves (Sennett, 2008). From this viewpoint effective pedagogies focus on development of tacit knowledge and can help students understand and engage in care that is more than technically correct. It is also concerned with the ‘how’ of caring (Frayling, 2012). Tacit knowledge is rooted in action and an individual’s commitment to their profession. This can be ‘more than the experienced practitioner can tell’ (Polanyi, 2009) and associated with expertise and mastery. The inexperienced practitioner
Whereas explicit knowledge is articulated and captured in text or drawing, tacit is not voiced, involves the senses, physical experiences and intuition. It consists of both cognitive (ability to perceive and define in the context of one’s world) and technical (know how) elements (Nonaka, 1994; Nonaka & Von Krogh, 2009).
It is this tacit knowledge that gives a practitioner the edge and helps them to advance in growing expertise but it can be difficult to uncover in others and to develop for oneself. There is an expectation that the learner picks this up in the course of work experience but it can seem mystical and unattainable to the learner (Frayling, 2012). Benner and associates (2012) in her skills acquisition model from novice to expert suggests that a mark of expertise is the ability to have an intuitive grasp on a situation which enables the nurse to know what must be done and how. She also advocates the use of pedagogical strategies that facilitate this development (Benner, Tanner, & Chelsa, 2012). Use of educational approaches as represented in the following model aim to help the student to recognise, ‘see’ and develop tacit knowledge which should help achieve this.
It is important to recognise that the proposed model was heavily influenced by a programme of research focused on uncovering what matters to patients and families. The specific details of the ways in which the model emerged from my work will become the subject of a future paper, so here I briefly indicate them to place my model in context. They included two studies set in the community care setting (Adamson et al., 2017; Cruickshank, Adamson, Logan, & Brackenridge, 2010) and the Leadership in Compassionate Care Programme (LCCP) (Edinburgh Napier University & NHS Lothian, 2012).The aim of the three year action research LCCP was to embed compassionate care in practice and education. The importance of tacit knowledge to enable and enhance person centered compassionate care was evident in all three studies The findings resonated with abilities of craftsmanship included in the model such as being curious, questioning, being open to do things differently, compassionate listening and connecting with the person as an individual (Dewar & Nolan, 2013; Edinburgh Napier University & NHS Lothian, 2012).
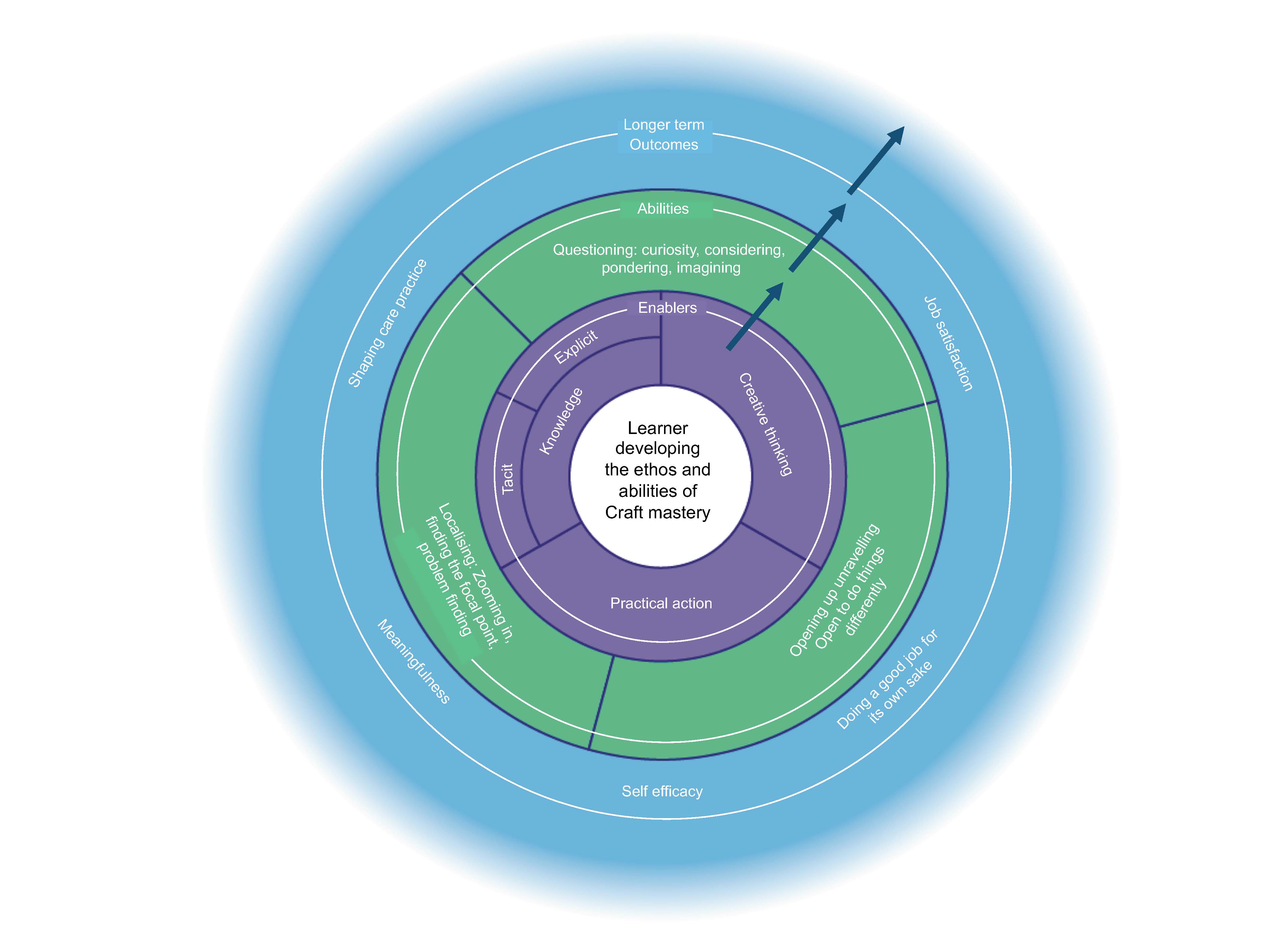
The first or inner ring within the model represents the learner; for whom the development of an ethos of compassionate craftsmanship via the overlapping surrounding elements is central. The second represents the enablers to the development of compassionate craftsmanship. The third circle represents the abilities that learners need to develop and apply in practice. The outer ring represents the anticipated beneficial outcomes that will influence care practice into the future. The arrows indicate progression.
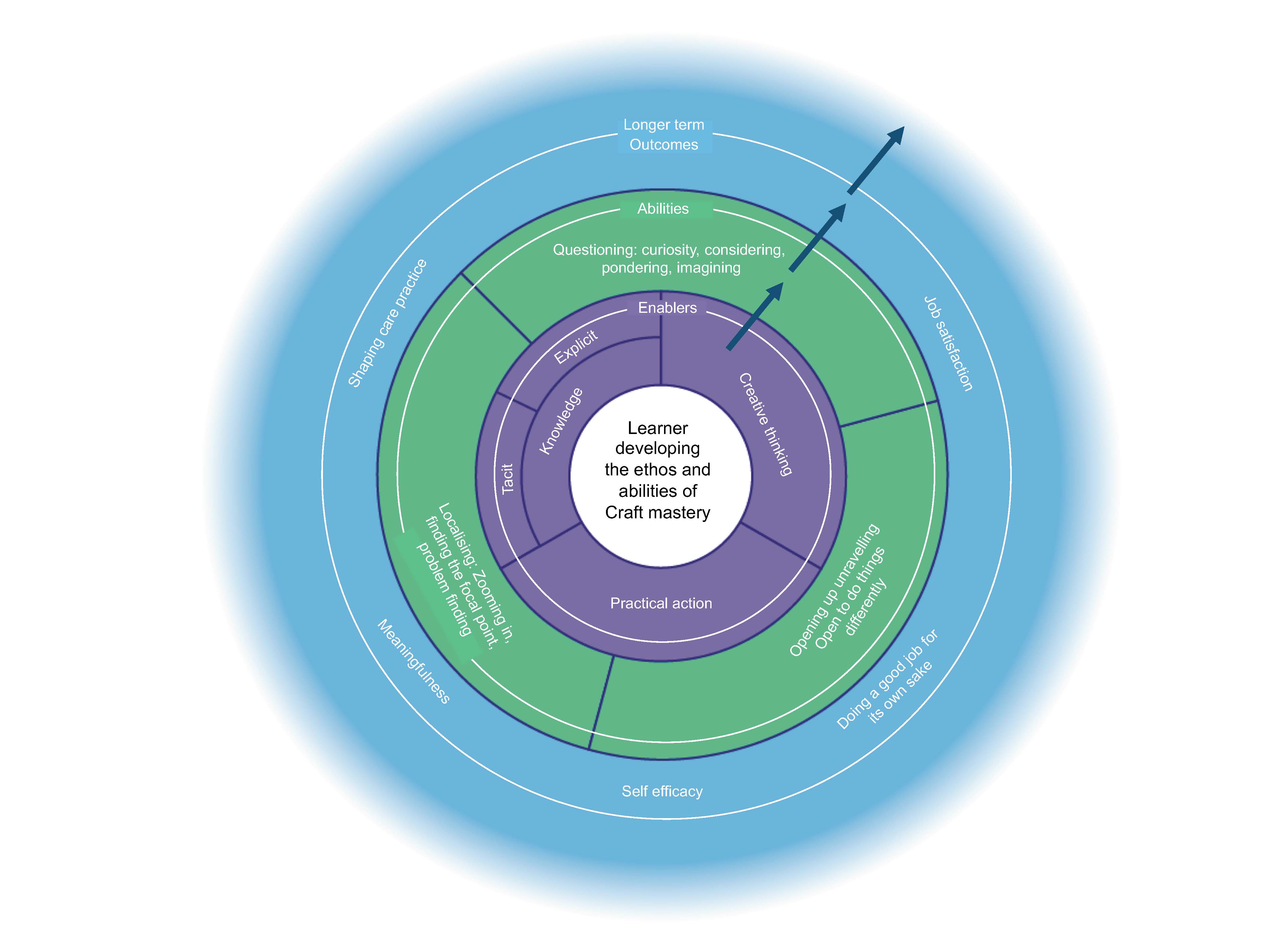
Figure 1: Model of Nursing Craftsmanship
The enablers are interrelated. The craft person engages in creative thinking through adoption of a creative mindset and continually seeks out and gains knowledge that is applied in practical action. The craftsperson attempts to make sense of a situation while allowing that sense making to be questioned and reshaped (Taylor, 2012). Therefore, pedagogical activities that encourage and enable the development and application of this mindset help the learner to keep an open mind, to consider alternatives and to imagine how things might be. As nurses they are seeking out and finding underlying problems and solutions through assessment and questioning (Sennett, 2008). The work of the nurse is social and Sennet suggests that the same capacity to influence is required for this as for the craftsperson working with physical materials (Meal & Timmons, 2012; Sennett, 2008). For this they require knowledge both explicit and tacit as well as flexibility to adapt to ever changing circumstances and each person as an individual.
The craftsperson uses knowledge to understand and overcome the constantly arising difficulties that grow out of variation in tools, materials and conditions in which they work. (Frayling, 2012, p. 78).
Sennet suggests three approaches to help students to develop the more difficult to attain tacit knowledge. The first approach he calls sympathetic Illustration which is focused on the needs of the learner. The lecturer shows empathy by sharing difficulties that they experienced as a novice including strategies to overcome these. These useful problem-solving techniques help the students develop their own strategies. This requires the expert retracing their practice step by step to the place before the activity became routine (Sennett, 2008). Use of loose analogies help the learner to feel that a new procedure/task is roughly like something they have done before and gain confidence to try to attempt the new. The student is encouraged to think creatively and imagine what engaging in a care activity or process might be like.
Secondly scene narrative acts as a vehicle for consideration of the ‘how’ of care by relating a story. It conveys the student to a scene clear in detail but puzzling in significance and meaning (Sennett, 2008). This is used to trigger curiosity and contemplation of what to do and how to do it. It encourages the learner to enter into the context and imagine what it would be like to be there. This is used to initiate independent thinking in the student, to help them understand the patient perspective and facilitates the development of creative thinking about care (Meal & Timmons, 2012; Sennett, 2008). One way to accomplish this is through sharing and reflecting on patient unique stories gathered in clinical practice (Adamson & Dewar, 2015), which can help students “stand in the patient’s shoes” (Browning, Meyer, Truog, & Solomon, 2007).
A third approach is instruction through metaphor which helps the student to consider the effect of an action, intervention or communication on person in their care. The student is encouraged to imagine for example the impact that a diagnosis may have on a person. One possible approach which could facilitate this and is through simulated practice in the classroom setting using simulated (actor) patients. Simulated practice environments are set up to mimic a real care setting and known to help students identify and even challenge their tacit values (Green & Bull, 2014). Students work in teams and are given a patient to care for or assess and provided with limited information about the person.
The aim is to encourage the learner to engage creative thinking in their situational problem finding and problem solving (Taylor, 2012). Opportunities for problem finding and problem solving which are closely connected in craftsmanship are woven into the learning experience.
The learner must uncover the often hidden problem and decide on and undertake appropriate care practices (take practical action), while observed by facilitators and peers (Carmel, 2013) who then feedback and initiate reflection and dialogue facilitated by the lecturer. Feedback from simulated patients is also valuable (Adamson & Dewar, 2011). In medical education this approach was found to help doctors reconnect with their humanness (Browning et al., 2007).
As learners are exposed to pedagogical approaches such as those described above it is anticipated that they will develop key abilities which are also interrelated. Those included in the second circle of the model are identified as foundational to craftsmanship (Sennett, 2008). These are firstly localising or zooming in on what is important; secondly the ability to question, to dwell on and ponder the situation or problem and seek solutions; and thirdly the ability to open up and unravel the situation or problem further. This is closely aligned with being open to act differently.
The practice of craftsmanship in nursing is mostly social (Coeckelbergh, 2014), as it requires connection and relationship with those with whom they work and with those for whom they care.
Localising relates to identifying the focal point and requires engagement of all of one’s senses (visual, auditory, tactile) in assessing, sensitive probing, compassionate listening and attending to clues so that key concerns can be identified and priorities decided. This relates to the nursing vigilance, awareness and attention to the needs of the patient (Grimley, 2017; Raingruber & Wolf, 2015).
Questioning draws on the tacit and requires the ability to think creatively. The craftsperson tries to make sense of the situation, is influenced by past experience but keeps an open mind. Sense making is questioned, reshaped and transformed (Taylor, 2012).
Opening up involves the craftsperson being open to do things differently, They apply fresh thinking and imagine an alternative way (Taylor, 2012). They are open to new ways of working and the views and suggestions of others. This may be patients and families as well as colleagues.
The ultimate aim is that the learner will grow in compassionate caring expertise and will experience the long term anticipated outcomes that feature in the outer circle of the model. These are also interlinked. The compassionate craftsperson needs to believe in their ability to provide compassionate care. Research shows that high self-efficacy is correlated with greater motivation and courage to attempt new and difficult tasks. Self-efficacious people also recover better from setbacks so important with increasing demands of healthcare provision. Research also shows that healthcare practitioners with low self-efficacy have been found to be less likely to exhibit compassion (Davin, Thistlethwaite, & Bartle, 2018). The craftsperson is committed to do a good job for its own sake (Sennett, 2008; Thorlindsson, Halldorsson, & Sigfusdottir, 2018), and take pride in their work (Frayling, 2012). Provision of compassionate person centred care is known to bring satisfaction and meaning for nurses (Dewar et al., 2014) and job satisfaction has been found to be closely linked to meaningfulness (Thorlindsson et al., 2018). Nurses who have this sense of meaningfulness of the work they do enjoy greater job satisfaction (Janssen, De Jonge, & Bakker, 1999; Raingruber & Wolf, 2015). The craft person who experiences these outcomes is well placed to influence and shape current and future practice. These links suggest that the anticipated outcomes could be seen as an interwoven whole.
In conclusion this model draws on the work of Sennett and others to present key dimensions of the development of nursing craftsmanship (Sennett, 2008). The interrelated elements of the model can prompt key questions and scaffold dialogue amongst educators and learners, about learning environments that inspire and engage learners in the pursuit of excellence and the invisible craftsmanship of compassionate caring. Its strengths are that it is student-centred and emphasises the importance of relational approaches to teaching and learning which can help students to begin to develop tacit knowledge so vital to the ‘how’ of caring practice.
Elizabeth Adamson is an Associate Professor in the School of Health and Social Care at Edinburgh Napier University. She has 19 years of experience in education both within clinical practice and higher education. l.adamson@napier.ac.uk